Adriaan Louw is a busy man. Between running ISPI (International Spine & Pain Institute), performing research, treating patients, drinking beer, and watching football he doesn’t have a lot of free time. However, he was kind enough to answer some quick questions to help me understand pain, central sensitization, and the clinical application of neuroscience. As always, his answers were very helpful and I thought I’d share them with everyone else.
I first met Adriaan when I took the NOI Mobilization of the Nervous System course. Check out my review of the course to catch up on some of the latest concepts. He is not only an extremely knowledgable clinician, but he is a very entertaining speaker as well. I cannot recommend taking a course with him enough. You’ll learn a ton, have a paradigm shift, and laugh a lot.
Adriaan is an expert on pain science and the clinical management of pain. He is also a Certified Spinal Manual Therapist and incorporates manual treatment with pain science to achieve the best results. He is a published author, lectures internationally, and recently completed his Ph.D. on therapeutic neuroscience education and spinal disorders.
11 Questions with Adriaan Louw
These questions are directed towards the clinical application of pain science. They will augment a background understanding of pain science and central sensitization.
1) You discussed a study in which just the mention of testing a nerve caused the subjects SLR to decrease due to anxiety. I’m having trouble trying to explain neurodynamics to my patients in regards to what I’m testing and what I’m treating. What type of language do you use for the peripheral nerve stuff?
• There are over 45 miles of nerves in your body. For normal function they glide and slide while we move. When nerves get hindered in their movement or become sensitive they tend to “tighten up” a little. The test we are doing is a way to see how easy your nerve can move; how far it moves and how sensitive it is. The treatment is a series of nerve glides to help the nerve move better and help calm it down (something like that).
2) What could be happening in those patients that perform exercises with no pain when they’re in the clinic with you, but then come back and report that they had a ton of pain at night? I know pain is an output, but if I can’t explain the mechanism I feel like I’m losing some “buy in” power.
• Latent pain can be from various aspects: Afterglow effect of inflammation – we know DJD increases inflammation with use, i.e., grandma walks ++ Christmas shopping, and pays for it that even when she gets home. With increased use – maybe a little inflammation, wakes up the nerves as the day goes on.
• Focus – busy during the day and when a patient sits still and thinks about it, becomes “aware” back hurts.
• Depending on work – back pain at work may not be an option for the brain – really need the job; rumors about layoffs, etc.
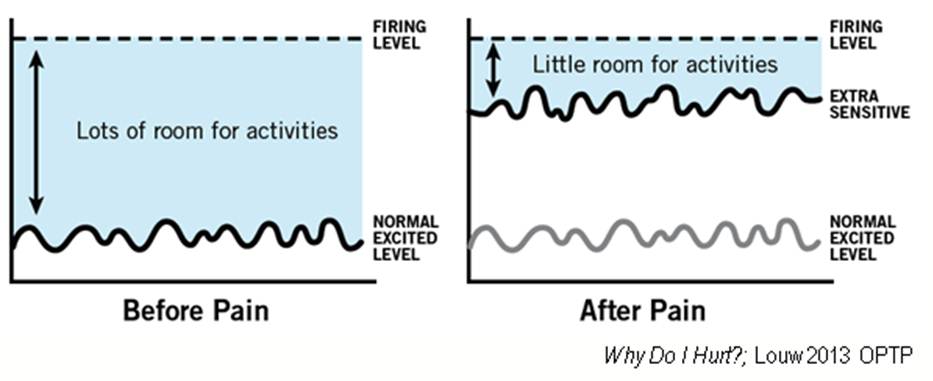
• Likely the way I will go: The alarm system (nervous system) gets activated throughout the day and steadily creeps closer to the threshold and at the end of the day – alarm goes off
• Obviously you will need to examine/ask and see which fits best. Bottom line – various reasons; we can explain it, and can make it better….
3) What could be happening when someone has no pain during the movement, but then pain immediately after they stop? I see this happen often in shoulders.
• Pain after muscle contraction
• Muscles heal in short amounts of time
• No/minimal pain during contraction = good; muscles = good
• 45 miles of nerve in the body; intertwined through tissue, including muscle. Contracting a muscle can also set of the neighboring alarm system – i.e., nerves. This may validate muscle is OK, but the adjacent nerves are extra sensitive and now you’re well on your way with pain education….Now the paradigm shifts to calming the nervous system down….
4) What is one of your favorite stories/examples to help patients understand pain. I often use the story you told us about the guy with leg pain that laid on a railroad track to self amputate and sill had pain after (phantom limb pain).
• I don’t think it’s a story as much as a metaphor that can easily be applied to them. Sure – a person cutting their leg off or hiker Aaron Ralston cutting his arm off is interesting, but not personal. Maybe your patient saw Kevin Ware earlier this year in the NCAA basketball tournament break his leg on national TV, but did not scream “pain” – but rather “win the game”
• My biggest “ah-ha” moments come with simple paradigm shifts like this:
• Suzy – if you sprained your ankle, would it hurt?
• Suzy – if you sprained your ankle, while crossing a busy street and a bus is coming straight for you, does it hurt? You can see the gears turning
• NO PATIENT has ever told me yes – obviously no
• We discuss:
• Bigger threat wins
• Pain is an output
• Tissue injury and pain are not the same
• I’ve had many people say: “So pain is a decision by the brain?”
• Now we’re heading down a neat and interesting path
5) What is one of your favorite metaphors to help describe the process of pain to patients?
• See above
• Another one: If you step in a rusted nail, do you want to know about it? – explaining nerve functioning as an alarm system, action potential, danger message to the brain and action taken.
• Another one: What would you do if a big roaring African lion jumped into this room right now? Stress response and multiple systems activating to protect you
6) What is the best way not to offend patients when you are basically telling them that their pain (or at least some of it) is in their head?
• Pre-empt it. Rusted nail example above – brain has to know there is a nail, so yes; it has to go to the brain. Is the pain in your head? Yes – but in your brain; in your head and biological and real.
7) I’ve had patients where I’ve tried to explain pain to them about a thousand times. No matter what approach I use, they won’t budge. I’m sure a big part of it is that I must not be explaining it in the best way for them to understand it. But what do you do in cases where someone refuses to believe anything other than that their tissues are causing pain?
• Cannot fix all. The art of therapy is matching the patient to the treatment and vice-versa. It’s no different than manipulating a patient and they get worse. Pain is complex and so many factors determine the outcome.
• If we find resistance, we don’t force it, but look for a back door. A recent patient wanted some trigger point therapy and “none of this cognitive nonsense you do here.” We did a thorough examination on her, set her up for some trigger point therapy and as she calmed (over a few sessions) we started educating her about pain while doing “traditional therapy.” Simple questions (nails; ankles sprains) and even the big ones” What do you think is going on with your neck?” “Why do you think therapy has not helped before?” etc.
8) What is the biggest mistake you see clinicians making when treating the nervous system (peripheral or central)?
• Several (sorry)
• They become nerve heads and believe everything is a nerve
• They view nerves as the “next” magic tissue. We’re bored with joints, muscles and fascia so we find the next magic “tissue.”
• Underestimate our ability to impact the nervous system and brain with novel therapies
• Overly aggressive – i.e., neural “tension”
• Forget the nervous system is an emotional, living, breathing organism in close contact with its cousins the immune system and endocrine system and ultimately attached to a 100 billion neuron brain!
9) What are your thoughts on chronic tendinopathies? We know that in these chronic tendinopathies there can be a histological change in tissue, dysfunctional healing, pain, and weakness (J Cook, P Malliaras, K Khan). Many recommend exercises that help stimulate and reorganize the tendon, even though they cause might pain. How do you treat this in your paradigm? Is explaining pain enough, or do you address the dysfunctional tendon tissue?
• Clockwise ultrasound
• I’m a nerve head – and I’ve read some neat stuff by Kharim Khan on this. All I know – the longer pain lasts, the more the nervous system, immune system and brain will be involved. BTW – tendons don’t cause pain – pain is 100% from the brain.
• Exercise may help pain, but is it purely due to its effect on the tendon?
• Treatment: The clinical issue – I will make sure the patient get’s a whopping dose of neuroscience education; strategies to help the physical health of the nervous system ALONG with the cool “tendon stuff.”
• We know you can think your ankle swollen. Any lasting pain causing a “worry” will lead to such an event and likely contribute – hence – a physically and emotionally healthy nervous system.
10) Pain science is really blowing up these days. It is really changing the way we approach pain. Both our profession and our patients are benefiting from it. However, some are such strong advocates of pain science that it seems like they’d prefer PT’s to treat their patients mentally on a couch rather than physically on a plinth. Where do you see our profession going with the new pain paradigm shift in the future?
• We cannot keep up with the university lectures we get invited to. I tell students very bluntly:
• Graduate
• Enjoy therapy
• Resent therapy
• Hit rock bottom
• Start drinking (or drink more)
• Seek a new paradigm – welcome to pain science
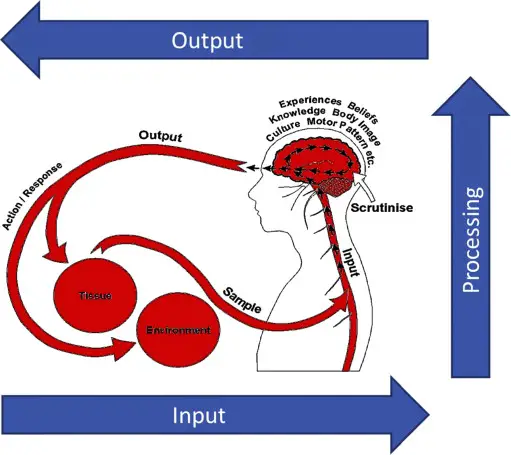
• Turner and Whitfield showed 97% of what a PT uses in his/her practice is based on what PT school taught them. If that paradigm embraces the Cartesian model of pain (pain and tissue injury is synonymous) you’re screwed. If your school has updated to the Pain Gate – you’ll be good at putting TENS units on patients, but Ron Melzack who designed the Pain Gate with Patrick Wall has taken us to the brain and The Neuromatrix, which is where we need to be; but don’t camp out there too long – people like Mick Thacker is taking PT to the immune world….and more.
• Paradigms change when you need them to change. Maitland (immense respect for him) worked for a while for me and sure helps many of my patients today, but the more chronic pain we see; the more a pain science or neuroscience view is needed.
• To answer the question:
• If a joint is stiff and a patient cannot move = PT’s job to treat the patient (mobilization and manipulation)
• If a muscle is not contracting and a patient cannot move = PT’s job to treat the patient (motor control)
• If a trigger point is causing loss of ROM and pain and a patient cannot move = PT’s job to treat the patient (trigger point therapy)
• Then – if a patient won’t move or exercise because they have bad beliefs (i.e., I have a bulging disc or arthritis), why does it become psychology? PT uses therapeutic neuroscience education to alter beliefs; reorganize the patient’s belief, they have less fear and move better….
• Putting all of this into perspective: I started in pain science in 1998 and 1/7 Americans had persistent pain. It’s now 1/3 = 100 million. No way of hiding this. Either learn about this or find yourself working at Lowes or Home Depot in the near future. (Make sure you lift with your legs; right……?)
11) There’s so much information out there that it can become overwhelming. Could you recommend some good places for people to go to learn more?
• Self serving: www.ispinstitute.com – courses, books, articles. We just launched a textbook Therapeutic Neuroscience Education with the aim of getting it into PT school.
• AAOMPT has some pain information
• IASP – world body on pain
• NOI
• Read this book: The Brain That Changes It Self
Dig Deeper
Books for Patient Pain Education
SomaSimple Adriaan Louw Interview
Sign up for ISPI Newsletters, it’s free quality information
BSMPG 2013 Summer Seminar (Video)
WCPT Congress – Focused Symposium: Pain Management (Video)
Research
—
The main reason I do this blog is to share knowledge and to help people become better clinicians/coaches. I want our profession to grow and for our patients to have better outcomes. Regardless of your specific title (PT, Chiro, Trainer, Coach, etc.), we all have the same goal of trying to empower people to fix their problems through movement. I hope the content of this website helps you in doing so.
If you enjoyed it and found it helpful, please share it with your peers. And if you are feeling generous, please make a donation to help me run this website. Any amount you can afford is greatly appreciated.




Adriaan is so fun to learn from. I just returned from the ISPI pain conference. If you weren’t there…WHY